Female Infertility
Primary female infertility means not being able to get pregnant for the first time after at least 12 months of trying (or 6 months if the woman is over age 35). Secondary female infertility is the inability to become pregnant or to carry a baby to term after previously giving birth.

The cause of female infertility can be difficult to diagnose.
Problems include irregular ovulation, hormonal disorders, damaged or blocked fallopian tubes, thick cervical mucus, or abnormalities of the uterus such as fibroids and endometriosis to name a few. If a woman keeps having miscarriages, this is also regarded as infertility.
Age is an important factor. From the age of 32, a woman’s chance of conceiving start to decrease, and from the age 35 that rate of decrease speeds up. Men aged 35 are half as fertile as they were at the age of 25, and from the age of 55, their fertility declines dramatically.
The cause of female infertility can be difficult to diagnose. It can arise from age-related factors, physical problems, hormone problems, and lifestyle or environmental factors.
In most cases of female infertility, there is a problems with producing eggs. In primary ovarian insufficiency, the ovaries stop functioning before natural menopause. In polycystic ovary syndrome (PCOS), the ovaries may not release an egg regularly or they may not release a healthy egg.
Common treatments include IVF, hormone therapy and if necessary, surgery.
While about a 30% of the time infertility is due to the woman, about 30% of the time it is the result of a problem with the man (sperm related or due to ejaculation/obstruction). In a further 30% of cases, the cause is due to both partners and the remaining 10% of cases the cause is unknown. This is called ‘unexplained’ or ‘idiopathic’ infertility.
It is recommended that most couples see a fertility specialist if they have failed to fall pregnant after 12 months of trying. If the woman is older than 35, reduce this to 6 months of trying. You should also see a specialist sooner if you or your partner have any known conditions or risk factors that may affect your fertility.
Your specialist will ask about how long you have been trying to conceive, how often you have sex and at what point during your cycle. They will also ask about your menstrual cycle and whether you have ever been pregnant previously.
Your specialist will take a full medical history, looking for any possible causes of fertility problems and perform a physical examination. Your specialist may then recommend tests to work out the cause of your fertility problems.
- Ultrasound of reproductive organs
- Ovarian reserve testing
- Estrogen level tests
- Prolactin level tests
- Genetic testing
- Blood work to test hormones
- Antral Follicle Count (AFC) ultrasound
- Saline Infusion Sonohysterogram (SHG)
- Smoking
- Drinking alcohol
- Obesity
- Being underweight
- Excessive caffeine intake
- Illegal drugs (including marijuana)
- Sexually Transmitted Diseases (STDs)
- Taking certain medicines
- Having previous treatment for cancer, such as chemotherapy and radiotherapy
- Doing regular, intense, strenuous exercise that results in your periods stopping
- Having certain underlying medical conditions, such as diabetes, thyroid disease or an autoimmune disease
Common causes of female infertility
There are also a range of factors that can cause female infertility. These include:
- Ovulatory disorders
- Polycystic Ovary Syndrome (PCOS)
- Recurrent Pregnancy Loss (RPL)
- Primary Ovarian Insufficiency (POI)
- Diminished Ovarian Reserve (DOR)
- Endometriosis
- Tubal factor infertility
- Fibroids
Treatments available for female infertility
Fertility drugs are the main treatment for women who are infertile due to ovulation disorders.
Fertility drugs assist by regulating or stimulating ovulation.
Other treatment options may include surgery to address any underlying condition, or assisted reproductive technologies (ART). Some common treatments include:
- Medical therapy (fertility drugs)
- Cycle tracking
- Tubal flushing
- Ovulation Induction (OI)
- Artificial Insemination or Intrauterine Insemination (IUI)
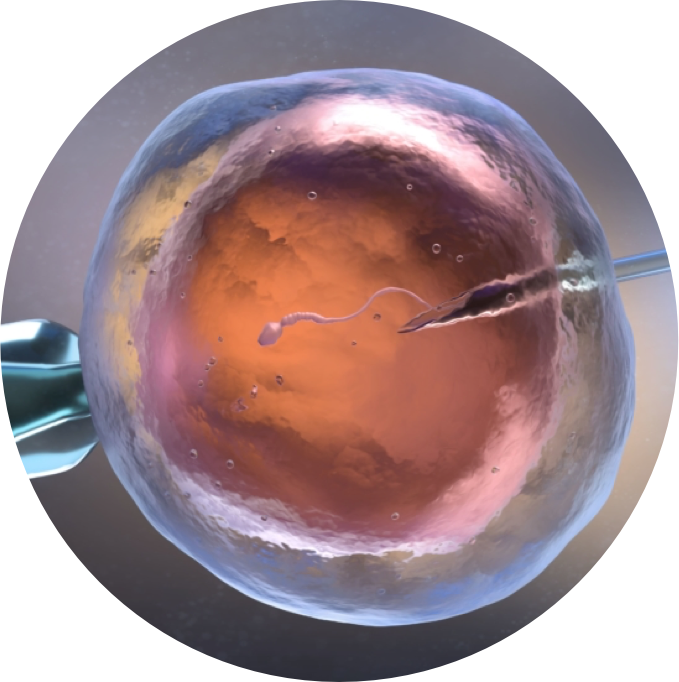
- In-Vitro Fertilisation (IVF)
- Intracytoplasmic Sperm Injection (ICSI)
- Male partner semen analysis to ensure he is fertile
- Laparoscopic “keyhole” surgery to address obstructions or underlying condition (fibroids, polyps, endometriosis, cysts, etc)
IVF is the most commonly used and the most effective treatment for female infertility. It is also the usually the first treatment recommended for women with blocked fallopian tubes.
IVF is generally performed at a specialist clinic. The treatment cycle involves taking hormonal medicine for several weeks to stimulate your ovaries to produce multiple eggs, which are then retrieved from your ovaries using a needle (under local or general anaesthetic). The eggs are put into a special dish in a laboratory and sperm is added to the dish to fertilise the eggs. Fertilised eggs that develop into embryos can then be inserted into your uterus after about 3-5 days.
Blood tests are taken after several days to determine whether the embryo has implanted in your uterus, forming a pregnancy.
If multiple eggs are fertilised, some of the embryos may be frozen so that they can be used later, if needed.
IVF success rates vary, depending on factors such as your age and the cause of your infertility.

Dr Shadi Khashaba is a sub-specialised fertility and reproductive medicine specialist. He is formally trained as a specialist obstetrician and gynaecologist, however he now focuses his clinical practice exclusively on fertility medicine.
Dr Khashaba has undertaken multiple sub-specialised training fellowships both domestically and internationally at renowned institutions in the areas of reproductive endocrinology, infertility, andrology and reproductive endocrinology.
He consults from the Sydney CBD, Alexandria, Kogarah and Miranda.
Get In Touch
If you have a fertility question or wish to make a booking, please contact us to find a convenient time and date. A GP referral is required.