Male Infertility
Male infertility is defined as trying without success to get pregnant for a period of 12 months, and you’ve been having sex at least twice a week.

Around 30% of fertility problems originate in the man.
The inability to conceive after 12 months affects about 17% of couples in Australia. Male infertility is a major factor in about 30% of cases.
Male infertility usually results from the obstructed passage of sperm, problems with quality of sperm (low numbers of poor strength) or hormonal problems.
Age is also an important factor. Men aged 35 are half as fertile as they were at the age of 25, and from the age of 55, their fertility declines dramatically. However, it is still possible for men as old as 70 to father children – it might just take longer to achieve.
Around 20 million sperm per millilitre (ml) need to be present in the ejaculate, with enough mobility and strength to swim the journey to the fallopian tube where conception normally takes place.
The odds of a young fertile couple conceiving by having sexual intercourse around the time of ovulation is approximately 20% every month. A couple isn’t suspected of fertility problems until they have tried and failed to conceive for 12 months.
In most cases, couples can be helped with assisted reproductive technologies (ART) such as IVF or even successfully resolved by their GP without the need for a specialist.
Despite popular belief, around 30% of fertility problems originate in the man. Another 30% originate in the woman and 30% are due to a combination of both partners. No cause is found in around 10% of couples investigated for infertility and this is called ‘unexplained’ or ‘idiopathic’ infertility.
It is recommended that most couples see a fertility specialist if they have failed to fall pregnant after 12 months of trying. If the woman is older than 35, reduce this to 6 months of trying. You should also see a specialist sooner if you or your partner have any known conditions or risk factors that may affect your fertility.
Your specialist will ask about how long you have been trying to conceive, how often you have sex and at what point during your partner’s cycle.
Your specialist will take a full medical history, looking for any possible causes of male fertility problems and perform a physical examination – including an inspection of your penis and testicles. Your specialist may then recommend tests to work out the cause of your fertility problems.
Your specialist will also want to know:
- If you experience sexual dysfunction (erectile dysfunction, premature ejaculation, low sex drive, etc)
- If you experience paid, discomfort, a lump of swelling in the testicle area
- If you have had previous groin, testicle, penis or scrotum surgery, including vasectomy
- Is your partner over the age of 35
- Semen analysis
- Blood test
- Urine test
- Ultrasound or MRI
- Testicular biopsy
- Genetic testing
- Karyotype testing
Common causes of male infertility
There are a range of medical factors that can cause male infertility. These include:
- Varicocele
- Infection (including STDs)
- Ejaculation issues
- Antibodies that attack sperm
- Anabolic steroids
- Tumours
- Undescended testicles
- Hormone imbalances (eg: insufficient testosterone)
- Defects of tubules that transport sperm
- Chromosome defects
- Sexual dysfunction (erectile dysfunction, premature ejaculation)
- Certain medications
- Prior surgeries (including vasectomy, prostate surgery)
Treatments available for male infertility
12.5% of infertile men have an easily treatable condition.
For these men, after basic treatment, often from their GP, they are likely to be able to get their wife pregnant naturally.
For those men who remain unable to achieve pregnancy, there are options to address the underlying issues. These include:
- Lifestyle modifications
- Hormone therapy
- Artificial Insemination or Intrauterine Insemination (IUI)
- In-Vitro Fertilisation (IVF)
- Intracytoplasmic Sperm Injection (ICSI)
- Surgery
Common conditions treated by surgery:
- Bloating of veins inside the testes (varicocele). This condition can be surgically treated.
- The tubes within the male reproductive system that transport sperm may be blocked, perhaps by injury or vasectomy. In some cases, the blockage can be surgically removed and the tubes repaired.
- If surgery doesn’t work, the man may undergo another surgical procedure called percutaneous epididymal sperm aspiration (PESA). Under local anaesthetic, a slender needle is inserted into the epididymis. Sperm are removed and either used immediately for IVF or frozen for later use.
The pituitary gland in the brain releases hormones called gonadotropins, which stimulate the testicles to produce sperm. In a small number of cases, male infertility is caused by insufficient levels of these gonadotropins. Taking these hormones as medication may boost sperm production.
The man’s semen is collected, washed and concentrated, then introduced into his partner’s uterus through the cervix.
This option may be chosen when:
- The concentration of sperm in the man’s semen is low
- The man has functional problems, such as impotence
- The man’s seminal fluid contains antibodies against his sperm
- The women’s cervical mucus is abnormal and it interferes with sperm transport.
IVF is the most commonly used and the most effective treatment for infertility.
In-Vitro Fertilisation (IVF) is conception outside of the human body. Sperm is collected from the man and is placed in a special incubator. The woman undergoes ovulation induction (hormonal stimulation of her ovaries) and eggs are collected. This is done through the vagina under ultrasound control.
The collected eggs are mixed with the sperm and they are placed in a special incubator. The fertilised eggs develop into embryos, which are then implanted into the woman’s uterus through a thin tube inserted through the cervix, again under ultrasound guidance.
IVF success rates vary, depending on factors such as your age and the cause of your infertility.
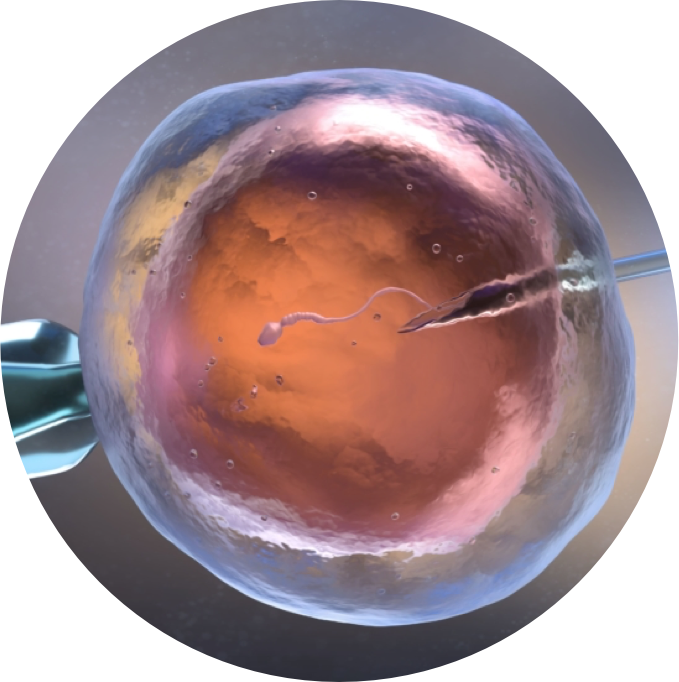
Sometimes, semen contains too few (or too few structurally normal) sperm to make fertilisation possible through IVF. Intra-cytoplasmic sperm injection (ICSI) can be used in these cases.
The eggs are removed from the woman’s ovaries and each is injected with a single sperm. The fertilised eggs develop into embryos that are transferred into the uterus at the appropriate time.

Dr Shadi Khashaba is a sub-specialised fertility and reproductive medicine specialist. He is formally trained as a specialist obstetrician and gynaecologist, however he now focuses his clinical practice exclusively on fertility medicine.
Dr Khashaba has undertaken multiple sub-specialised training fellowships both domestically and internationally at renowned institutions in the areas of reproductive endocrinology, infertility, andrology and reproductive endocrinology.
He consults from the Sydney CBD, Alexandria, Kogarah and Miranda.
Get In Touch
If you have a fertility question or wish to make a booking, please contact us to find a convenient time and date. A GP referral is required.